Detailed Analysis of the Contribution of CSF Metabolomics Schizophrenia
Schizophrenia is an ill-defined, complex psychiatric disorder that runs in about 1% of the world’s population. It manifests in delusions, hallucinations, disturbances in cognitive functions, and emotional blunting, which makes it quite difficult to diagnose and treat. In all honesty, though the causes of schizophrenia are yet unknown, research into neurobiology, genetics, and biochemistry only supports the depth of their understanding of the disorder. One promising area is cerebrospinal fluid metabolomics, which involves an advanced method through which it analyzes the metabolite profile around the brain and the spinal cord of cerebrospinal fluid.
Here, we will review the expanding interest in CSF metabolomics schizophrenia spectrum in its potential to identify clinically relevant biomarkers and to shed light on disease mechanisms guiding new therapeutic strategies.
What is CSF Metabolomics?
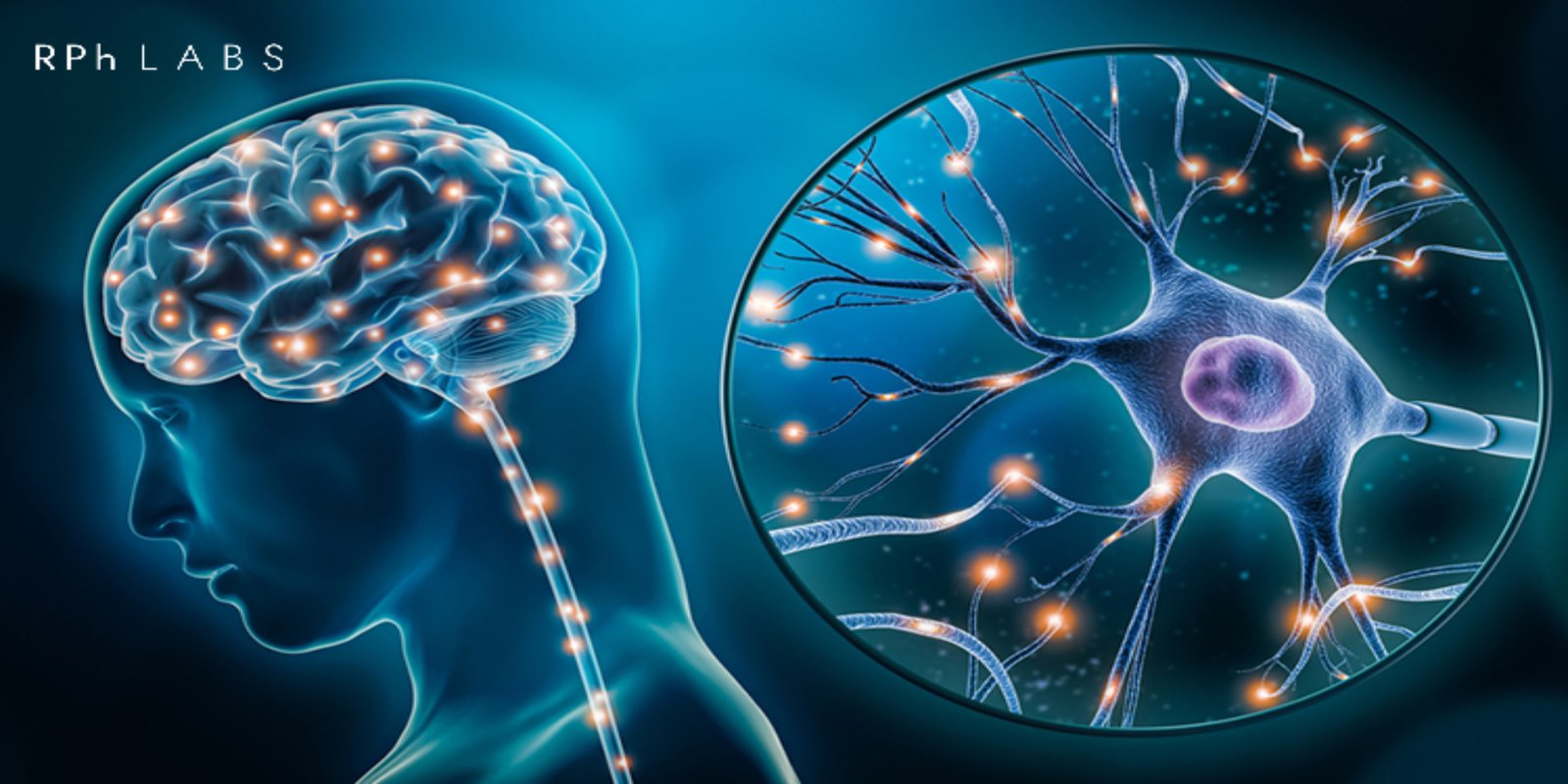
The comprehensive study of those small molecules produced during metabolism within biological systems is metabolomics. The end products of gene expression and cellular activity represent the metabolites, giving an impression of the metabolic state of a person. Metabolomics of CSF directs attention to the metabolites within the cerebrospinal fluid bathing the brain and spinal cord.
CSF is particularly helpful for research because it reflects the biochemical environment of the CNS, thereby explaining the nature of brain metabolism, neurotransmitters’ function, and neuroinflammation. One can obtain CSF by performing a lumbar puncture or spinal tap through which one can study metabolites that are more directly related to both brain activity and pathology.
CSF samples contain a wide range of metabolites that can be identified and quantified using mass spectrometry (MS) or nuclear magnetic resonance (NMR) spectroscopy. Metabolites identified include amino acids, lipids, organic acids, and neurotransmitters, all of which are very relevant for indicating critical aspects of brain health and disease processes.
Role of CSF Metabolomics Schizophrenia
The deranged neurobiological pathways have been associated with schizophrenia, and it has been known to be related to the disturbed neurotransmitter systems, including dopamine, glutamate, serotonin, and cellular energy metabolism. It is one of the scientific tools that can discover such pathways. This would, in turn, cast light on possible biomarkers for diagnosis, prognosis, and therapeutic targets.
Neurotransmitter Dysfunction
Characterizing schizophrenia is dysfunction in neurotransmitter systems, particularly the dopamine, glutamate, and GABA (gamma-aminobutyric acid) ones. Such neurotransmitters have previously known key roles in mood, cognition, and sensory processing. A level of signaling change has been related to the pathophysiology of schizophrenia.
Dopamine:
Dopamine dysregulation has been considered central to the positive symptoms of schizophrenia, primarily hallucinations and delusions. CSF metabolomics studies suggested the potential link in dopamine system pathology through the imbalance of dopaminergic metabolites, such as homovanillic acid (HVA).
Glutamate:
Glutamate is considered to be the most crucial excitatory neurotransmitter in the CNS, and its receptors, particularly the NMDA receptors, are implicated as being central in synaptic plasticity and cognition. Reduced NMDA receptor activity has been considered to be one of the central etiopathogeneses for the observed cognitive deficits that are associated with schizophrenia. Metabolomics studies also suggested changes in glutamate and other closely related metabolites, like glutamine, in the CSF of patients with schizophrenia.
GABA
GABA is the most potent inhibitory neurotransmitter and synchronizes with excitatory neurotransmitters to maintain a balance. The cognitive and sensory processing deficits seen so vividly in schizophrenia have been the dysregulation of the GABA system. Metabolomic profiling of CSF may identify changes in GABA levels or its metabolic byproducts.
Energy Metabolism and Mitochondrial Dysfunction
A hypothesis is emerging suggesting that schizophrenia may be associated with disorders in the energy metabolism of the brain, primarily because of mitochondrial dysfunction. Mitochondria are generally known as the powerhouses of cells, as they provide the energy source necessary for cell functioning in the form of ATP. Mitochondrial dysfunction reduces the productivity of ATP and floods neural Tissue with disrupted energy in the form of damaging oxidative stress.
Metabolomics of CSF detected disturbances in the metabolism of compounds associated with mitochondrial functioning, which include aberrantly altered levels of lactate, pyruvate, and acetylcarnitine that could be caused by alterations in cellular energy metabolism. Other abnormalities of concentration of other metabolites, such as creatine and phosphocreatine, that are involved in the ATP buffering system, were detected in the CSF of schizophrenia patients, and these could propose impairments of energy homeostasis.
Inflammation and Immune System Activation
Neuroinflammation is increasingly being raised in the pathophysiology of schizophrenia. Immunity response and inflammation metabolites could be traced by CSF metabolomics. The concept is exemplified by a tryptophan metabolite kynurenine produced through the pathway of tryptophan degradation. There has been established an increase in the concentration of schizophrenia, indicating that this is an immune system’s altered response. The kynurenine pathway has neurotoxic metabolites, thereby affecting the brain’s function.
Levels of pro-inflammatory cytokines are increased in the CSF of schizophrenic patients, and changes in the metabolites related to oxidative stress and inflammation are researched intensively for potential use as biomarkers for the disease.
Oxidative Stress and Antioxidant Defenses
Schizophrenia is characterized by increased oxidative stress, a condition of imbalance that results from the overproduction of free radicals and a failure to neutralize them. Oxidative stress might affect the cell lines in the brain because it causes neuronal death, blunting neurotransmitter systems. The oxidative stress markers are MDA and 8-OHdG, with the body’s antioxidant defenses, including glutathione, which can be determined using metabolomics from CSF.
Biomarkers for Diagnosis and Prognosis
The most exciting application of CSF metabolomics in schizophrenia research is to uncover potential biomarkers for diagnosis and prognosis. Perhaps the identified biomarkers using metabolomics might be useful to make distinctions between schizophrenia and other psychiatric diseases, prediction regarding the onset time of the disease, or follow-up monitoring for the progression of symptoms.
Examples include, for instance, a metabolite signature in CSF that may predict schizophrenia before it appears clinically to enable early intervention and improve its prognosis. Another example is that the profiles of metabolites could predict which patients would probably respond to a given treatment and hence guide the therapy through a personalized approach.
Challenges and Future Directions
Although it shows much promise, there are some significant challenges to be overcome in the future with CSF metabolomics:
- Standardization: Among the biggest challenges posed is the lack of standardized procedures in the collection, processing, and analysis of samples. Metabolite profiles can be produced based on any number of factors, like diet, medication, handling biological samples, etc.
- Heterogeneity of Schizophrenia: Schizophrenia is a heterogeneous disorder, implying that different subtypes of the disease may have different underlying metabolic signatures. That renders it more difficult to identify universal biomarkers.
- Ethical and Practical Problems: To obtain CSF, the patient must undergo an invasive procedure, which might limit this data in large-scale clinical studies. The ethical issue of obtaining samples of CSF from vulnerable populations, such as those suffering from severe mental illness, also persists.
Despite these challenges, the future is bright for CSF metabolomics in schizophrenia research. With the availability of modern technology, advancement in data analysis, and finally, an enhanced understanding of the disorder, metabolomics could take a crucial role in improving diagnosis, treatment, and outcomes among schizophrenia patients.
How PGx Testing Benefits Schizophrenia Treatment
- Selection of drug-continuation: Many variations in CYP450 and other enzymes contribute to the metabolism of drugs, their effects, or side effects. PGx testing of RPh Labs enables the selection of the most appropriate drug. For example, risperidone vs. clozapine.
- Avoidance of side effects: Many variants of genes like CYP2D6 or DRD2 act as predictors of side effects such as sedation, gain in weight, or movement disorder for better selection towards the safety of the drug used. PGx Gene test will help avoid such side effects.
- Tailor-made Doses: Pharmacogenetic testing characterizes a slow or fast drug metabolizer, allowing doctors to administer the doses in time to avoid toxicity or ensure efficiency.
- Enhanced Compliance: The toxicity and effectiveness of the drugs are improved with Pharmacogenomic testing, thus improving adherence in patients.
Conclusion
CSF Metabolomics Changes Our Perception of Schizophrenia CSF offers an extremely high-resolution biochemical profile of the environment of the brain. The study of the metabolites present in CSF has revealed insights into neurotransmitter dysregulation, energy metabolism, neuroinflammation, and oxidative stress mechanisms, all relevant to schizophrenia pathophysiology.
Given the fast-moving nature of research in this area, CSF metabolomics may prove of enormous potential for early diagnosis, individually tailored therapy, and deeper clarification of molecular underpinnings of schizophrenia. There is a lot of scope yet to be realized regarding this approach to reshaping schizophrenia research and clinical practice.
Leave a Reply