
Introduction
Postural Orthostatic Tachycardia Syndrome (POTS) is a dysfunction of the autonomic nervous system, which controls involuntary processes like heart rate, blood pressure, digestion, sweating, and temperature regulation. Is POTS Genetic? No, there is no scientific evidence of genetic mutation leading to this disorder; however, evidences show that some people, following a family history of POTS, are at higher risk of catching this condition.
- Key feature: rapid heartbeat when standing. Other symptoms include dizziness, syncope, POTS syndrome, fatigue, brain fog, and exercise intolerance.
- This is predominant in individuals aged 15 – 45, especially women, who are strangely affected (approx. 80%).
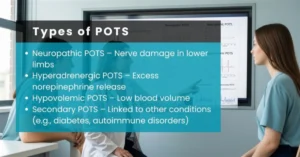
Types of POTS
The following are the three main types of POTS; there are more subtypes which have not been included herein:
- Hyperadrenergic POTS: The most prevalent among POTS, about 60% of all cases. Standing causes norepinephrine to go high, causing palpitations, tremors, and anxiety.
- Neuropathic POTS syndrome: Small fiber nerve damage impairs blood flow to the legs, leading to blood pooling in the legs and lightheadedness.
- Hypovolemic POTS: Associated with extremely low blood volume, Hypovolemic POTS reduces cardiac output, worsening symptoms like dizziness and fainting.
- Secondary POTS: Linked to other conditions (e.g., diabetes, autoimmune disorders)
Postural Orthostatic Tachycardia Syndrome (POTS) is a condition whose etiology is still unclear. This condition has numerous underlying causes, out of which, one prominent reason is lack of blood (Hypovolemia).
Is POTS Genetic?
- Evidence indicates POTS is rarely familial, with most cases being irregular.
- As per Hopkins Medicine, no single gene mutation has been definitively linked to POTS.
- Some familial clustering exists, suggesting a possible predisposition, but this is uncommon.
POTS and Ehlers-Danlos Syndrome (EDS)
- Individuals with hypermobile EDS are at higher risk for POTS.
- Coexisting Ehlers-Danlos Syndrome (EDS) may increase the severity of postural orthostatic tachycardia syndrome symptoms.
Moreover, EDS patients experience excessive flexibility (looseness) of connective tissue, which may impair vascular tone (network of blood vessels), contributing to orthostatic intolerance, a condition characterized by symptoms such as lightheadedness, sweating, nausea, anxiety, and even unconsciousness. Orthostatic intolerance is a different condition that drops your blood pressure upon standing, whereas in POTS, your heart rate increases upon a change in position.
Hypovolemic Syndrome Explained
- Hypovolemia means reduced blood volume, often due to low plasma volume.
- Hypovolemic syndrome worsens (limits) blood in the lower body, triggering tachycardia (high heart rate) and dizziness.
- Treatments focus on increasing fluid and salt intake, sometimes using fludrocortisone or midodrine to boost circulation.
Experiencing mental health issues?
Most mental health medications tend to affect people differently. Pharmacogenomics testing (PGx testing) gives clear insights into genetic makeup, allowing doctors to tailor drugs and dosages.
Book an at-home PGx test from CLIA-accredited RPh LABS now and discover how you may respond to over 250 medications.
Mechanisms Behind POTS
- Norepinephrine overactivity: Seen in hyperadrenergic POTS; high levels cause rapid heart rate and anxiety.
- Peripheral denervation: In neuropathic POTS, nerve damage reduces vasoconstriction in the legs.
- Autoimmune and inflammatory triggers: Some cases follow viral infections or autoimmune disorders.
- Secondary triggers: Surgery, trauma, or prolonged immobility can precipitate POTS.
POTS Symptoms Checklist
- Rapid heartbeat upon standing
- Dizziness or lightheadedness
- Fatigue and brain fog
- Syncope POTS syndrome (fainting episodes)
- Palpitations, tremors
- Exercise intolerance
- Panic attacks, due to overactivation of the sympathetic nervous system, which is responsible for the ‘fight or flight’ response of our body.
POTS Syndrome Treatment:
While there are no POTS syndrome treatments yet, management of this syndrome is possible.
Lifestyle and non-pharmacologic:
- Hydration (2–3 liters/day)
- Salt intake (5–10 g/day unless restricted).
1 teaspoon on level is approx. 6g of salt. - Compression garments to reduce blood pooling
- Gradual exercise (recumbent cycling, rowing, swimming)
Medications:
Although the FDA has approved no POTS medications, your doctor may suggest you some off-label medication, including;
- Beta-blockers to reduce heart rate
- Fludrocortisone to increase blood volume
- Midodrine for peripheral vasoconstriction
- Pyridostigmine for autonomic support
- Individualized approach: Type-specific management is critical, e.g., hyperadrenergic POTS may respond better to beta-blockers, neuropathic POTS to midodrine.
Natural Approaches to POTS
- Consistent hydration and electrolytes
- Gradual aerobic conditioning
- Avoid triggers like prolonged standing, heat, or alcohol
- Mindfulness and paced breathing for POTS and panic attacks
Prevention and Long-Term Management
- No guaranteed prevention exists.
- Early recognition and structured lifestyle adjustments reduce symptom severity.
- Regular monitoring, hydration, and exercise improve long-term quality of life.
| POTS Type | Key Mechanism | Recommended Treatments | Notes / Tips |
| Hyperadrenergic POTS | Excess norepinephrine on standing → rapid heart rate, palpitations, anxiety | – Beta-blockers (e.g., propranolol) to control heart rate- Low-dose clonidine in some cases- Increased salt and fluids- Gradual exercise (recumbent first) | Avoid stimulants (caffeine, decongestants). Monitor BP closely. |
| Neuropathic POTS Syndrome | Small fiber nerve damage → poor blood return from legs | – Midodrine to constrict blood vessels- Compression stockings- Salt and fluid loading- Recumbent or seated exercise | Focus on improving venous return. Elevate legs during rest. |
| Hypovolemic POTS | Low blood volume → insufficient cardiac output | – Fludrocortisone to expand plasma volume- High salt and fluid intake- Compression garments- Recumbent exercise | Monitor electrolytes regularly. Gradually increase activity levels. |
| Mixed / Other Forms | Combination of the above mechanisms | – Tailored combination of above treatments- Lifestyle changes (hydration, salt, exercise)- Medications based on dominant mechanism | Requires close follow-up with neurologist/cardiologist. |
Additional Practical Tips for All Types:
- Keep a daily symptom and heart rate log to track triggers.
- Avoid prolonged standing and hot environments.
- Small, frequent meals can prevent postprandial hypotension, which worsens POTS symptoms.
- Consider mindfulness, paced breathing, or therapy if anxiety or POTS and panic attacks occur.
Conclusion
Postural Orthostatic Tachycardia Syndrome (POTS) isn’t just passed down through from your forefathers to you. Still, genetics might play a part alongside triggers like environmental factors, autoimmune issues, or lifestyle habits. Spotting POTS symptoms—such as dizziness, a fast heartbeat, or constant tiredness—is key to getting diagnosed and starting treatment early. With the right medical advice, lifestyle tweaks, and therapies, you can take control and improve your day-to-day life with POTS. Researchers are diving deeper into its genetic roots and causes, which could lead to better, more personalized treatments down the road, giving hope to everyone managing this condition.
Frequently Asked Questions
Currently, no reports confirm that POTS is genetic; however, prevalence in people with family history is higher.
No, POTS is not a disease but an autonomic nervous system disorder causing rapid heart rate and orthostatic intolerance (increased heartbeat, headache, anxiety, sweat, or anxiousness upon standing).
Yes. A cardiologist or a neurologist may diagnose POTS. Diagnosis involves heart rate monitoring, tilt-table testing, and blood pressure assessment.
Yes. POTS can cause sympathetic nervous system overactivity, which is responsible for the ‘fight or flight’ of our body; thus, not only anxiety, but also POTS and panic attacks may be possible.
Disclaimer: This blog is for informational purposes only and does not constitute medical, legal, or professional advice. While we strive for accuracy, errors or omissions may occur.
Leave a Reply